Accreditation in Healthcare- Role of Nursing Sensitive Quality Indicators
The current trend in healthcare is encouraging organizations to acquire ‘accreditation’ with national (NABH) and international organizations (JCI). The process not only helps the institution to demonstrate quality patient care, understand lacunae, scope of improvement but also enhancing their reputation as healthcare providers.
Accreditation in Healthcare– What does it mean?
Accreditation is granting recognition or certification to an institution that maintain defined benchmark standards. Accreditation in healthcare happens through a review process where the healthcare organization is allowed to demonstrate their ability to meet regulatory standards.
Who defines the standards?
Usually the healthcare organization have to meet the standards that are defined by a recognized accreditation organization for example:
Joint Commission International (JCI)- Joint commission international is one of the relied upon international accreditation body known for its standards and stringent quality evaluation process. Learn more about JCI here:
https://www.youtube.com/watch?time_continue=82&v=19ffgRFCt8Y
National Accreditation Board for Hospitals & Healthcare Providers (NABH)- It is the Indian accreditation body established to operate the accreditation program of health care organizations. Learn more about NABH here:
How does accreditation help?
In Healthcare, accreditation has multiple benefits. It influences organization, patient and the professionals like nurses as well.
1. Benefits to the Patient- Patient gets quality care from credentialed professionals where patient satisfaction is given preference and their rights are respected.
2. Benefit to Healthcare Organization- Healthcare organization gets to keep abreast with the benchmark standards, ensuring quality care with increased confidence of the society in the services provided by the organization.
Click to know more:
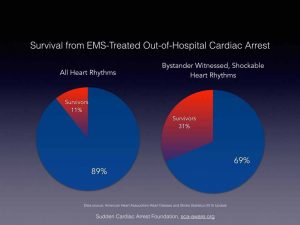
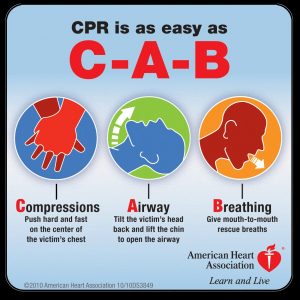
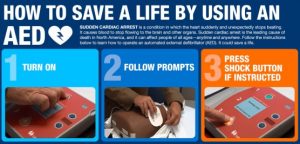
3. Benefits to Healthcare professionals- Healthcare professionals’ credentials are part of the assessment process during the accreditation process. It ensures that the professionals are updated and also checks that there competency is assessed periodically. For example nurses need to be trained in performing CPR and must be given a chance to update through in-service education.
To learn more you may enroll for the CPR course here: /product/cardio-pulmonary-resuscitation-cpr-adult/
Role of Nursing Sensitive Indicators during Accreditation
Quality indicators as such are important to achieve the target of getting an organization accreditation. Though the review of literature presents a complex picture, quality indicators are very important to enhance the quality of healthcare services undergoing accreditation process. Nursing sensitive indicators generally refers to various aspects of nursing care including the following:
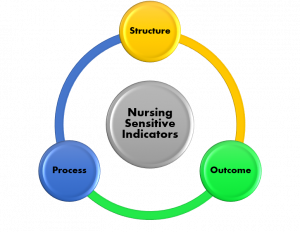
1. Structure Indicators- These include nursing manpower, competency or skill level of nursing staff and education as well as certification levels of nursing staff.
2. Process Indicators- Includes patient assessment methods and nursing interventions.
3. Outcome Indicators- These refer to outcome of patients depending upon the quality of nursing care provided such as patient fall, pressure ulcers, infections and patient satisfaction with nursing care.
During the accreditation assessment process all these aspects are assessed for nursing professionals.
Improving the Nursing Sensitive Indicators- Getting ready for the Accreditation!
As a nurse leader, one often faces challenge to allocate and manage resources ensuring the quality of care a patient receives. Let us learn about what you can do as nursing professionals to focus on structure, process and outcome standards which you may be asked about during the accreditation process and how to prepare yourself for that in advance.
Structure Indicators
- Nursing Manpower- Nursing manpower is crucial and a difficult area to conquer. It is forte of the HR and chief of nursing together. To ease the efforts and to follow the league as nurse leaders try the advance tools available. One such system is acuity based staffing. Such systems are based on patient requirement. For example a nurse can be allocated to one, two or multiple patients based on needs with patient categorized as dependent, semi-dependent and independent. Learn more about staffing here:
- Skill assessment– Nursing skill assessment is done in many organization periodically by education department. However, in India, competency based assessment is very limited. Do note that accreditation agency look out for these parameters.
- Certification and Continuing education- The education team has to often present the record of nursing staff during the accreditation. The staff nurses might be picked up randomly and the records may have to display in front of the auditor. Nurse educators often struggle to reach every nurse for updating them. Switch to online education for easy access and record maintenance. This can help you as educator to track the progress of individual nurses and also provide flexibility to the nurses to learn at their own pace and anywhere they want. Follow the link to know more: https://bodhilabs.ai/product-category/nursingcourses/
Process Indicators
- Patient assessment methods and nursing interventions- Patient assessment methods should be relevant but should not overburden the nurses. The purpose of assessment methods is to ensure minimize the loop holes in care provided to the patients. A measure to ensure quality care by the nurses. Nurses must be involved in the care assessment pathways developed for the patient care. Latest addition to the care pathways is to develop decision support systems which not only guides the nurses what to assess but what action they must take next. Follow the link to know more:
Outcome Indicators
These indicators are the most crucial Nursing Sensitive Indicators as these are directly related to patient outcome.
- Patient Fall- Patient fall is one of the most dreaded incident on the list of a clinical nurse as well the whole caring team. Fall can cause internal injury, laceration, fractures and bleeding. Studies show that about ‘one-third’ of the hospital falls are preventable. Especially in elder population fall can be important cause of mortality and morbidity. Causes are many including previous history of fall, drugs, and other causes such as visual disability or neurological impairment. Assessment tools are available and must be used by nursing professionals to avoid the events.
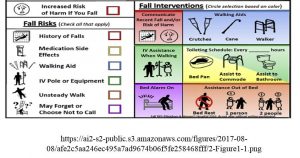
Centre for Disease Control (CDC) has proposed fall prevention program called STEADI (Stop Elderly Accidents, Deaths and Injuries). Follow the link to know more: STEADI Pocket Guide
STEADI tool kit for Healthcare Providers:
- Hospital Acquired Pressure ulcers (HAPU)- HAPU indicates the poor quality of care in a healthcare set up. Especially if the pressure ulcer progresses to stage 3 or 4, it can cause infection, mortality and morbidity and also increases the length of stay of a patient.
Florence Nightingale in 1859 wrote:
“If he has a bedsore, it’s generally not the fault of the disease, but of the nursing”
Though it has been supported by many studies that the entire team (doctors, nurses, physiotherapist and dietician) is responsible if a patient develops pressure ulcer but it largely falls on the shoulders of nursing team. Assessment is the key to prevention for most of the outcome based quality indicators. Braden scale is reliable and popular scale used in healthcare setting to assess the risk of pressure ulcer as development of pressure ulcer is affected by many factors. Here are the components of Braden scale.
Learn how to assess stages of pressure ulcers. It is very important that nurses look out for patient vulnerable surfaces every day and pick early signs of pressure ulcer.
Stage I pressure ulcer- It is characterized by intact skin with non-blanching erythema.
NOTE: This is an important time to identify pressure ulcer and many professionals fumble about identifying the stage I pressure ulcers. If the nurses are careful to document there are chances that the pressure ulcer is detected only when it reaches stage II.
How to test for Non-blanchable erythema- The classic sign of Stage I pressure ulcer?
- Apply light pressure on the suspected area for few seconds
- Release and watch for return to usual skin color
Blanchable- Skin color returns immediately to normal. See blanchable skin.
NOTE- it is normal response.
Non-blanchable- Persistent redness or rashes in lightly pigmented skin. See how you can identify non-blanchable
erythema to label it as LEVEL I PRESSURE ULCER.
Stage II pressure ulcer- Pressure ulcer turns into an open ulcer involving epidermis, dermis or both.
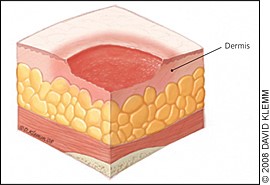
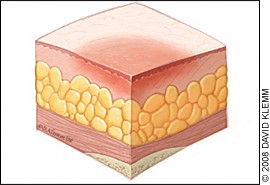
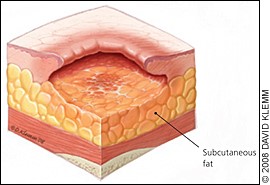
Stage III pressure ulcer- It involves full-thickness tissue loss with visible subcutaneous fat.
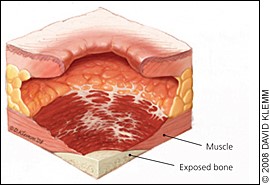
Stage IV pressure ulcer- In stage IV the pressure ulcer has involves underlying muscle and bone.
See link to know more about staging, back care and management of pressure ulcer here:
https://bodhilabs.ai/product/care-of-patient-with-pressure-injury-bed-sore/
- Central line associated blood stream infection- A central line-associated bloodstream infection (CLABSI) is infection that occurs when organisms enter the bloodstream through the central line.
CDC recommends the following precautions for health professionals to prevent CLABSI:
- Perform hand hygiene.
- Apply skin antiseptic.
- Ensure that the skin preparation agent is completely dried before inserting the central line.
- Use maximal sterile barrier precautions including sterile gloves sterile gown, cap, mask and sterile drape.
- Once the central line is placed follow recommended central line maintenance practices. Wash hands with soap and water or an alcohol-based hand rub before and after touching the line
- Remove a central line as soon as it is no longer needed.
- Also find the checklist proposed by CDC called the CLABSI bundle.
https://www.cdc.gov/hai/pdfs/bsi/checklist-for-CLABSI.pdf
- Catheter Associated Urinary Tract Infection- Urinary tract infections account for 40% of all hospital-acquired infections and 80% of such infections are known to be associated with indwelling urethral catheters.
CAUTI Prevention- Nurses must consider the following points when planning to insert a catheter.
- Insert catheter only when indicated. Consider other options such as condom drainage or intermittent catheterization.
- Ensure that only trained professionals insert the catheter. You may access the course here:
- Follow sterile technique during insertion of catheter.
- Minimize days of insertion. Remove catheter as soon as possible.
- Maintain close drainage system.
- Practice hand hygiene and standard precaution during patient care.
Learn about Nurse driven protocol to reduce CAUTI by Joint Commission International (JCI) for free:
Restraints- Use of restraint in hospitalized patient especially in ICU patients is practiced is listed as a nursing quality indicator by National Database of Nursing Quality Indicators in US. Many times it becomes difficult to avoid the use of restraints but it is always suggested that restraints be used as a last resort when patient poses threat to self or others.
Types of Restraints-

Physical restraints- These restraints restrict or control the movement or behavior. These include hand mittens, belts, bed rails, lap cushions etc.
Chemical restraints- These restraint control the movements or behavior through medications such as tranquilizers and sedatives.
Nursing responsibilities when a patient is prescribed restraints:
- Observe patient every 15 minutes for the first hour of restraint and subsequently as per the age every 2 hourly or 4 hourly.
- Assess physical condition of the patient including, vitals, hydration, nutrition, and joints of extremities being restraint, comfort of the patient and hygiene needs.
- Psychological status and need for further revision of orders.
- Assess patient for continuous need for restraint and patient behaviors during temporarily removal of restraints.
- Special care should be given to the area where the restraint is applied example hands must be assessed when using wrist restraint or mittens as restraints for any injury resulting from the restraint.
Outcome indicators must be monitored, documented and reported by each team of a unit in the healthcare setting and measures to improve the outcomes must be discussed and implemented in consensus with quality team and nursing team to achieve the goals as a team to improve patient care using the recent evidence based practices. The whole process is usually a matter of interest for the treating team but also for the accreditation agencies to track the progress an organization makes to ensure quality care to a patient which generally goes by the name of ‘Root cause analysis’ by the quality team.
Conclusion
Nursing sensitive quality indicators are a must to be monitored in any healthcare organization as it is a direct measure of nursing care in an organization, also it pushes the healthcare team to perform better in addition plays a crucial role about reflection of best practices in an organization during the accreditation process. Learn more about NABH accreditation Nursing Excellence Standards here:
https://www.nabh.co/NURSINGEXCELLENCE.aspx
References:
1. Heslop L, Lu S. Nursing-sensitive indicators: a concept analysis. J Adv Nurs. 2014 [cited 2019 Feb 28]: 70(11); 2469–2482. doi: 10.1111/jan.12503.
2. The Sentinel Watch. The three types of nursing indicators. 2011 Nov 2 [cited 2019 Feb 28]. Available from: https://www.americansentinel.edu/blog/2011/11/02/what-are-nursing-sensitive-quality-indicators-anyway/
3. Almoajel AM. Relationship Between Accreditation and Quality Indicators in Hospital Care: A Review of the Literature. World Applied Sciences Journal. 2012 [cited 2019 Feb 28]: 17 (5); 598-606. Available from: https://pdfs.semanticscholar.org/581c/5fbb1fa8e12ecbf6feb8989ba499b02d0162.pdf
4. Nightingale F. Notes on nursing . Philadelphia: Lippincott; p. 1859.
5. Cuddigan J. Stage 1 Pressure Injury: Non-Blanchable Erythema of Intact Skin. National Pressure Ulcer Advisory Panel. 2017 Mar 3 [cited 2019 Mar 3]. Available from: https://www.npuap.org/wp-content/uploads/2017/03/Cuddigan-Janet-Stage-1.pdf
6. Salamon L. Catheter-associated urinary tract infections: a nurse-sensitive indicator in an inpatient rehabilitation program. Rehabil Nurs. 2009 Nov-Dec [ cited 2019 Mar 3] :34(6); 237-41. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19927851
7. Registered nursing.org. Use of Restraints and Safety Devices: NCLEX-RN. Available from: https://www.registerednursing.org/nclex/use-restraints-safety-devices/