Burnout among Nurses- Is it for Real?
“This is a disaster!” Mike said.
“May be you shouldn’t take your laughs so seriously” said Sully (Mike’s best friend)
“But – I- I mean, work has been-” Mike tried to explain that he took his jokes very seriously..
A story about the best laugh collector (Mike) inspired from the movie “Monsters, Inc.” The best laugh collector forgets how to laugh himself, taking his job too seriously, spending lesser time with family and friends. But thankfully he was confronted on time by his friends about what he was doing to himself.
Burnout is a term used very commonly to describe simply the amount of stress someone is undergoing these days. But is this phenomenon that simple? Is it same as stress? Read on to understand how burnout might spread across an organization if left untreated as any contagious disease. There are studies that indicate that if someone around you suffers from burnout, it is likely that you might get affected. In fact, a study indicated that nurses who reported highest prevalence of burnout among their colleagues were more likely to experience high level of burnout themselves.
Story of a highly competent Nurse
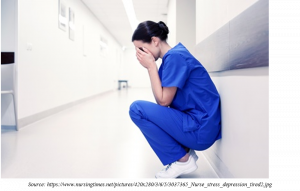
Ms. N graduated from a premier institution of the country where she got exposure to the best of the facilities, mentors and clinical exposure. She had learnt from the best and seen the most challenging cases. She graduated and joined a private hospital as an ICU nurse. Within months of her service she was assigned mostly the difficult cases and was often called on off days as she was one of the most competent nurses. Her unit was busy, working hours mostly exceeded and she sometime even skipped her break time to manage the patients. Over time, she developed back pain and suffered problems of GI track. At home, she would often eat unhealthy as she would feel exhausted all the time and was unable to cook. She would hardly go out or talk to anyone. As time passed she started to fall sick more frequently. One day she did a major medication error but patient was thankfully saved with timely intervention. She applied for a leave and did not return to work for a week. Later, it was found that she had locked herself in the house and did not interact with anyone including friends and family. She took quite a long time to join back.
Nursing Burnout not only impacts the nurses but also the patients and the organization for which they work. In fact, nurses who suffer from burnout are more likely to leave their jobs creating yet another reason for staff shortage which might create a vicious cycle of more nurses falling prey to burnout.
Is Stress same as Burnout?
Stress and Burnout are not the same. However, stress in combination with other factors might lead to burnout.
Stress is the response of body to any internal or external stimuli. Peculiar it might sound I am sure if you are health professional and reading this, you might have heard of ‘good stress’ or ‘Eustress’. As a student I was quite fascinated by this term and it is ingrained in my memory forever. Eustress is a positive response to perceived threat or stressor which is known to enhance once performance. The figure below explains simply how stress might affect an individual.
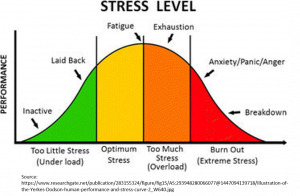
As it is rightly pointed, burnout occurs as a result of too much stress and happens over a period of time. An individual if exposed to constant stress will eventually suffer from burnout.
What is Burnout syndrome?
Burnout syndrome is a prolonged response to chronic emotional and interpersonal stressors on the job. It affects an individual on physical, mental and emotional level. The term ‘syndrome’ is frequently attached rather than calling it simply burnout as the individual suffers from group of symptoms and burnout affects more than one system of the body.
The three dimensions of burnout
Maslach Burnout Inventory is often used to assess the level of burnout an individual is undergoing. As per this there are three important scales that can define burnout.
- Emotional exhaustion- It refers to the feeling of being emotionally overextended and exhausted by one’s work. You must have come across someone around who is emotionally exhausted. For example a previously enthusiastic colleagues appears really dull, anxious or is easily irritable.
- Depersonalization- It is the impersonal response of the individual towards patients/others. The person has callous or cynical attitude. For example blaming a patient for the disease or dropping an insensitive comments on colleagues.
- Personal accomplishment- It is the feeling of competence and successful achievement in one’ work. The individual with sense of reduced personal accomplishments feels insufficient in terms of work he/she performs and has poor professional self-esteem.
Burnout syndrome is characterized by increased emotional exhaustion, increased depersonalization and reduced personal accomplishment.
Learn more about Stress and Burnout here:
Assess your burnout level with this burnout self- test here:
https://www.mindtools.com/pages/article/newTCS_08.htm
Risk factors of Burnout
Though burnout is mostly associated with work related stressors but personal attributes also impacts how prone a person is to burnout. Following are some of the risk factors associated with burnout.
- Age- Age has been indicated to be associated with burnout. Some studies say that the burnout increased with age where as some say otherwise. Meta-analysis of studies indicate that age is inversely associated with burnout that is younger nurses are more likely to undergo burnout as compared to their older counterparts. Read more here: https://onlinelibrary.wiley.com/doi/pdf/10.1002/nur.21774
- Gender- Female nurses are more at risk of burnout as compared to male counterparts.
- Marital status- Single or divorced individuals are at higher risk of burnout
- Number of children- Having no children is found to be associated with higher risk of burnout
- Level of education- Studies indicate that higher the level of education, more are the chances of an individual to suffer from burnout.
- Work hours- Nurses’ job is often a difficult one, in terms of working hours. Sometimes, it is not even a choice for nurses to take double shift with staff shortage being an issue in healthcare. Nurses working in busy areas not only miss their breaks (which is required physically as well mentally) but also go overboard to extend work hours without even being paid for the extra hours.
- Work setting- Challenging settings such as those nurses who work in emergency or ICUs are at higher risk of developing burnout.
- Perfectionism- A nurse who is idealistic and is a perfectionist is at higher risk of burnout as such individuals are stressed if the work is not done as per their satisfaction.
- Over commitment- Someone who takes commitments very seriously and goes beyond role definition can undergo emotional exhaustion and develop burnout more easily.
- Work life balance- It is important to have work life balance to keep anyone sane. Often nurses witness a lot of disturbing things at work place which they do not wish to discuss at home. This could create a lot of stress as piling up things and not able to discuss with anyone about it.
- Unhealthy copying strategies like alcohol or drugs- Use of alcohol, drugs or unhealthy eating habits like refined products not only impacts the physical health but also mentally. Drugs or alcohol can affect the way mind thinks and can lead to serious mental disorders.
- Lack of support system outside work- Lack of support system can worsen the prognosis of burnout as the victims may not themselves understand how different they might start behaving.
Symptoms of nursing burnout
Know that if you have the following symptoms, you should stop and be aware that you might be heading towards burnout.
- Social isolation- If you have decreased social interaction and go out less to see friends and family, stop and understand that it is important to socialize. Additionally, if you are loner there is chance that you could be an easy prey to burnout. Studies indicate whether it is on purpose or due to exhaustion, loneliness impacts psychological and physical health.
- Sense of constant exhaustion- Nurses sleep cycle is often disturbed due to odd working hours and getting good sleep can be a problem. But if you observe that you have disturbed sleep pattern and you feel tired rather exhausted all the time, you might be falling victim to burnout.
- Change in habits- Eating unhealthy, eating less or more than your usual self, trying to relieve stress by unhealthy habits on a regular basis, stop doing something which you use to love doing may indicate burnout.
- Frequent sickness- Suffering from flues, stomach infection, back aches, headaches or inability to concentrate frequently indicates exhaustion.
- Emotional instability- Being resistant to change, anxiety related to new changes at work, crying, being indifferent to patients or colleagues might be some of the responses of a nurse suffering from burnout.
- Hate your job- While at some point of time all of us feel that we do not want to work if suffer a difficult situation. It is quite common to face such situations in healthcare. A nurse has to take a lot of human interaction which could be not so pleasant at times like explaining an anxious relative why his patient is not recovering or breaking bad news that a patient might never be able to walk again. But if you don’t like going to work and have this constant feeling every day what you are doing at this place reveals that you are stressed. There is less satisfaction, sense of achievement at work and more errors in patient care.
- Work phobia- If you constantly feel anxious about going to work or keep thinking about it even if you are not on the job or you feel that you are no more confident doing your routine job assignments, you need to stop and re-think why is it so? Were happy going to work earlier and now you don’t? There is possibility of burnout creeping in.
How to prevent nursing burnout?
Nursing burnout is a serious problem of the nurse as well as the organization he/she works at, as burnout impacts the quality of care a nurse provides hence impacts patient outcome as well as the overall performance of an organization.
If you are a nurse, practice following simple techniques to prevent burnout.
1. Trust yourself- If you feel you need to stop and you are not feeling well, stop and re-think. Think about what you are doing and ask questions if you have started doing something differently lately. Call in for a mental break.
2. Listen to those who care- Friends and family are often the first ones to notice the change in you. Listen to them. Find a work buddy with whom you can talk about work.
3. Eat healthy and exercise- If you are exercising without the necessary nutrition in your body, it may lead to more weight gain and fatigue to the body. Include as many colors in your food from fruits, vegetable, legumes, grains and avoid refined products.
4. Take short breaks- At work stop when you are feeling overwhelmed. Go for short tea breaks and consider it a mental break. Think it as a break from work and enjoy the time. Make deliberate efforts to find some time for yourself especially if you are a workaholic. And instruct yourself not to think about work when you are on a break. It will help in two ways. One, you will not worry too much. And two, you will come back with a fresh mental frame and perform better.
5. Practice relaxation techniques- If you are not an avid yoga follower, try practicing simple breathing exercises when you are feeling stressed.
6. Pursue a hobby- Easy it may sound, a difficult one to do. Try pursuing what you like doing like reading a book, swimming, dancing or playing a sport. Physical activities are recommended as it freshens your mind by releasing happy hormones like endorphins.
7. Be assertive- If you think you are unable to work in a particular area as it is taking toll on your health and you feel you’re heading for a burnout, talk to your supervisor and request a change.
8. Job change- An extreme step but if your job is too demanding and with all the efforts you have put in if you are still uncomfortable in the environment you work, consider a job change. This is a drastic step but if you ignore it for too long it might cost you your health and career. I recently came across an article where a person who suffered from burnout decided to quit the job, she talked to others who left the organization before she did and they told her that it was brave of her to stay for so long. The employer had unrealistic expectation and caused a lot of stress to the employees. So, it may not be you, if the work load is too much to handle with interpersonal conflicts a grave problem, it isn’t a bad idea.
Responsibilities of employer to prevent nursing burnout
- Set clear expectations from the nursing team.
- Lack of reward, control, clarity of role and support in an organization cause emotional exhaustion and depersonalization in an employee. It is the responsibility of an employer to periodically interact with employees to understand the individual goals. In bigger organizations the supervisors must take care of those working under them. Supervisor must stand by the nurses working in the unit in terms or working conditions and resources available to them.
- Acknowledge the contributions of the nurses periodically. It could be monetary or in terms of promotion, role change or an opportunity to grow such as through educational advancements.
- Plan time outs for the team like picnics or arrange indoor games like table tennis or outside easy to play games like badminton.
- Provide facilities that genuinely address the needs of the employees. For example majority of the nursing task force is still female. Arranging a crèche facility for the nurses’ children. It will keep them stress free as they can reach their children not so far away. Many multinational companies and certain hospitals have tied up with crèche facilities that are subsidized for the employees.
Conclusion

I will end this topic with the famous expression about the glass filled with water. Oh no, not talking about how you look at the glass, half empty or half full that tells how optimistic you are.
If the glass is half full (which shouldn’t be that heavy) but you keep holding it for hours, what will happen?
Your hand will start to ache… And if you hold the glass for days?
The hand will be numb and you will feel paralyzed.
Stress is like holding a glass of water. If you keep holding it, the end result is burnout…
So don’t carry it around, remember to put the glass down!
References:
1. Disney 5 minutes stories. Mike’s laughing matter. Disney Enterprises, Inc. 2012.
2. MedAptus. Is physician and nurse burnout contagious? 2019. Available from: https://www.medaptus.com/physician-nurse-burnout-contagious/
3. Mindgarden. MBI: Human Services Survey for Medical Personnel. Mind Garden Inc. 2019. Available from: https://www.mindgarden.com/315-mbi-human-services-survey-medical-personnel
4. Cañadas-De la Fuente GA, Ortega E, Ramirez-Baena L, De la Fuente-Solana EI, Vargas C, Gómez-Urquiza JL. Gender, Marital Status, and Children as Risk Factors for Burnout in Nurses: A Meta-Analytic Study. Int J Environ Res Public Health. 2018 Sep 25;15(10). pii: E2102. doi: 10.3390/ijerph15102102.
5. Jackson SE, Schuler RS. Preventing Employee Burnout. AMACOM. 1983. Available from: https://smlr.rutgers.edu/sites/default/files/documents/faculty_staff_docs/PreventingEmployeeBurnout.pdf
6. Glass of water. Emotional intelligence at work. 2015 April 1. Available from: http://www.emotionalintelligenceatwork.com/resources/fun-games/
