How can the healthcare providers improve retention of nurses and their job satisfaction?
“By 2030 India will need 6 million nurses and the global demand of healthcare workers will rise up to 80 million
-World Bank
It has been quoted a zillion times that healthcare cannot survive without nurses yet we fight to hold on to the nurses in most organizations. We would need millions of nurses by the end of the decade but are we taking steps to resolve the issue?
It puts in immense pressure on healthcare management as well as it topples the healthcare team which struggles to train and fit members in their team with much effort.
Top Reasons why Nurses Leave
Staffing and Workload
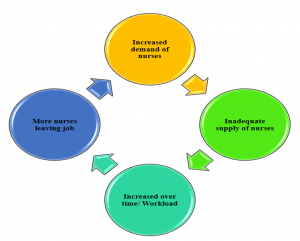
Balancing the nursing matrix can give nightmares to not only the nurse leaders but the top leaders of an organization. But, the solution isn’t that easy. Staffing issues and high workload are reported to be the topmost reason why nurses chose to leave the job. It is a kind of a vicious cycle!
Workload is not easy to define. It can be multifaceted how we can classify workload for nurses.
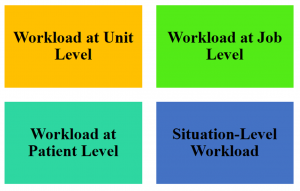
It could be workload at the unit level where the nurse-patient ratio is not right. Or it could be workload in terms of what type of job role a nurse has. For example, researches indicate that nurses who work in an ICU setting or emergency areas are prone to feel stressed due to the high workload and urgency of the situation.
Other patient level workloads may include ineffective communication which might result in a bad day for the nurse or lack of adequate stock supplies which might bother her/him as the work gets hindered. Situational workload might arrive unannounced many times even when a nurse is serving in so called ‘easy’ areas like wards (which are absolutely NOT). In fact, ward nurses might suffer from lack of supplies more frequently than ICUs and emergency areas counterparts which are rather luxurious in terms of supply. Every area where a nurse can possibly work has its own pros and cons.
You decide who is better off??
An ICU nurse who might not have to attend to patient attendants that frequently since communication protocols are well defined about how and when to pass the information, they are sorted. The nurse is assigned one or two patient at a time depending on the patient’s condition. But they deal with sicker patients, patient needs frequent monitoring and nurses hardly get a break to eat, hydrate or pee.
A ward nurse who has stable patients, who need no constant monitoring or need to be checked frequently and given medications only at routine intervals. The nurse is assigned four to six patients (sometimes even more) in one shift. She has additional responsibilities like attending rounds moving from room to room, attending to problems of patients and attendants, responding to call bells and list goes on…but something in common among ward and ICU nurses that is nurses hardly gets a break to eat, hydrate or pee.
So, here I have just put up two common scenarios but the challenges in other units where nurses work whether it is an OPD, diagnostics department or daycare, the problems are similar due to staffing issues which leads to increased workload.
Any comments yet about who is better the ICU ‘star’ or the ward ‘runner’?
Eventually in the hope of a better work environment, staffing or lesser workload nurses ‘Move’.
Job satisfaction
Simple it may sound, the word has multidimensional aspects to it. Job satisfaction has different definitions at different phases of work service. For example, a new nurse might not be satisfied with her/his job as she/he is unable to settle in, maybe she/he is not given much support or so-called ‘orientation’ or is overwhelmed as she/he is never seen such a setting before. I have personally interacted with many nurses who shared their concerns much later after the orientation phase. Some of them had never seen a ventilator machine before. Blame game won’t work, such people do enter the system.
Contrarily, if you talk to a senior nurse, who is in the middle management, the problems may emerge such as too much workload, carrier stagnation, issues with team members or work-life balance. So, ‘one size fit all’ approach might not work to sort the problems of nurses in general.
A study done in Coimbatore, India on nurses revealed that factors like age, nativity, support from family members, monthly income, place of stay, marital status, experience and tenure of job impacted the job satisfaction.
Pay and Benefits
As per May et al, increasing the wages to solve institutional workforce recruitment and retention problems is an easy-to-implement intervention in the short run. It can also not conclude about nurses’ outcomes such as nurse burnout, job dissatisfaction and intent to leave. Nurses in India still fight for wage difference between private and public sector.
Work-life imbalance
Missing in most of the professions of the world, nurses and health professionals were probably the first few, who were always pushed to boundaries to finish work or rather keep serving the patients without giving much thought about their personal lives. It is hard to maintain a work-life balance in healthcare as the demand-supply graph is skewed.
A new nurse is ‘utilized well’ by the supervisor in double shift many a time. And with monetary incentives, it is often compensated. But, these practices tend to take a toll on the patient and nurse herself/himself physically, mentally and socially. I came across nurses who would attend continuing nursing education programmes after night duties and I used to wonder what exactly are they going to learn from such sessions? So by doing so we are also shattering the individual need of a nurse to ‘learn or grow professionally’.
An experienced nurse, on the other hand, is caught up in a different direction. Though she/he may not be doing double shifts but she/he is made to stay longer sometimes to finish her/his assignments or to attend those management meetings which does not fit in her/his work timings and disturbs her/his family life.
Result in both case is frustration. It builds up and eventually leads to burnout where nurses no more care or they leave their jobs in the hope of a better work environment and culture. In this case, the role of nurse leaders and administrators is immense. Encouraging, appreciating the efforts as well as simple actions such as relieving the staff on time counts. So, think next time before you are keeping someone beyond their work time, everyone wants to go home!
Work environment
Initially, once a person settles in the job, it might appear to be a cakewalk but once you start interacting with the team, not only the nursing team but the others who contribute directly or indirectly in patient care like physicians, physiotherapist, nutritionist, ward assistants, they all start to matter. And these are significant factors that can make a nurse stay on the job.
A study by Duffield reported that a nursing manager who was perceived to be a good leader, was visible, and consulted staff, provided praise and recognition and offered flexible work schedules was a great factor found to distinguish the positive and negative working units.
A survey by People element shows reasons, why people leave the job. Interestingly, ‘Staffing and workload’ tops the reason in each phase of tenure when the nurses leave the job.

Other reasons cited why nurses leave the job
- Lack of role/job clarity
- Not valued
- No recognition or rewards
- Lack of career opportunities
An Indian study highlighted the difference in job stressors that might impact the retention of nurses in the public and private sectors.
Private hospitals
- Over duty and excessive timings
- Feeling of exploitation
- Low salary and slow increments
- Heavy work pressures
- Physical exertions with less or no breaks
Public hospitals
- No recognition
- Monotonous nature of job
- Peer issues
- Danger and legal exploitation by patients
- Less technical knowledge leading to job dissatisfaction
The Big Question- How to retain Nurses?
The scenario in India is changing for better (at least in the government sector). The demand is everywhere. Nurses are better paid now and are also encouraged to progress professionally through in-service initiatives and sponsorship for career progression. But we need to catch up in private sector. The work wages are still shameful to even disclose and other factors like workload and overload remain prevalent in private sector.
So What can administrators do?
The problems are different so the solution will have to be set based on the need. Some steps can be taken by the management to make a stronger bond with the nursing task force.
Support Nurses

Support to the nurses can come in many forms.
Welcome the new members- New nurses are often vulnerable due to lack of experience, newness to the settings in addition to the apprehension of what and how she is going to shine. Many hospitals follow a ‘mentor or buddy program’ that might help the new bees to settle in and orient them to the atmosphere. ‘Transition to Nursing Practice’ is what is being followed for safer practice and better adaptation of nursing students to transform into confident nurses. Below is a useful link to such practice.
Here is an excellent link that takes a nurse stepwise through a defined area where she/he might practice as a nurse.
https://www.qni.org.uk/nursing-in-the-community/transition-community-nursing/transition-gpn-toolkit/
Show that you ‘care’- This may reflect in the appraisal process and acknowledging the immediate efforts put in by the nurses.
Listen to them- Often nurses as a community feel that they are not heard. Here, the role of top leaders is to ensure that the nurse representatives and genuine, communicative and good problem solvers rather than the one who creates more hurdles for the group. Leaders can also encourage open sessions.
Positive work culture

Work culture tremendously impacts whether a nurse stays or goes out of the system. The study by Cowden T, reflects that there is a positive relationship between transformational leadership, supportive work environments and staff nurses’ intentions to stay in their current positions.
Incentive to Stay
An organization can set examples with a different approach through monetary and non-monetary incentives they might offer to nurses.
1. Flexible timings- As per Becker et al, nursing professionals are putting a demand of flexible timing due to varied reasons like aging nursing force, staff shortage and work-life balance. In such a case, chances of retention and staying back of experienced professionals are quite good.
A study with Flexibility!
- The nursing staff expressed the desire for more flexible rostering and the opportunity to work 12-hour shifts.
- After an agreement was reached between the hospital, the union and the Industrial Relations Board, guidelines were put in place and a Flexible Rostering System was proposed and trialed.
- Initially, the trial was conducted for three months and extended to six months.
- The shifts trialed were between 4- 12 hours in length with varied starting and finishing times.
- The Flexible Rostering System was evaluated using feedback from staff surveys and the results of a staff vote.
Outcome
- Positive with over 80% of staff voting to implement the Flexible Rostering System permanently.
- Reduction in sick leave by 41%.
- Improved retention of skilled registered nursing staff.
- Both patients and nurses commented on the improved continuity of care.
- Salaries and wages were within budget.
- Staff surveys showed positive feedback such as increased morale, increased flexibility with rosters, decreased fatigue levels, improved patient assessment on night duty and an increase in the number of days off.
2. Rules to protect nurses- with the massive number of cases coming to light every day about abuse against health professionals, administrators must work on stricter policies and rules to protect nurses. Several incidents have come to light and must be taken seriously. Usually, grievance policies are defined clearly but are the nurses aware? Make sure such policies are put to light clearly.
3. Clear job responsibilities- It might sound trivial but conflict might arise if the job roles are not defined properly. For example in many private set up ‘non-nursing tasks’ are defined and are taken over by the nursing assistants. But in India, we are yet to define them for the whole nursing community. It saves the precious time of a nurse and she/he can provide better quality patient care. As an administrator, poke your nose and know your nursing department inside out, to perform better as an organization. If you have a positive team of top and middle-level nursing managers who listen to their nursing team and communicate well with you, there is nothing better you can ask for.
4. Career opportunities- Often in government hospitals in India, a nurse can pursue her career further without losing her/his job but we hardly see such opportunities in the private sector. The same step might not be possible or practical but as an organization, encouragement to participate professionally or involve in conducting professional events like conferences, workshops might encourage nurses and allow them to showcase the work they do differently every day.
Fair Staffing

The most difficult step and a daily headache for the middle-level nurse leaders is staffing. Listening to the demands and not giving into the pressure by a specific unit (just because the head of department is bossy) is the key ?. A strong headed nurse leader can only do that and that is why it becomes all the more important for the administrator to pick leaders wisely.
Continuing Education on Current Updates
A well informed and skilled nurse is motivated and happy to work. Allow innovative ways to come into the learning system. Often, we see nurses are pushed to attend classes due to many reasons like requirement of quality initiative, policy of the hospital to name a few but you might also find some units where nurses happily attend the sessions. So, plan the session as per the interest, area where they work and introduce something that is challenging to keep their interest from fading away. Try online learning methods which will allow them to learn at their own pace.
Other interesting ways of learning like role-playing, case analysis and skill review sessions for newer technologies can also be helpful. See the link to know more.
Click on the link below to see some inspiring ways to retain your nurses.
References
1. Liu JX, Goryakin Y, Maeda A, Bruckner T, Scheffler R. Global Health Workforce Labor Market Projections for 2030. World Bank Group. 2016 Aug. http://documents.worldbank.org/curated/en/546161470834083341/pdf/WPS7790.pdf
2. Homburg V, Van der Heijden B, Valkenburg L. Why do nurses change jobs? An empirical study on determinants of specific nurses’ post-exit destinations. J Nurs Manag. 2013 Sep;21(6):817-26. doi: 10.1111/jonm.12142. Epub 2013 Aug 16.
3. Carayon P, Gurses AP. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.
4. May JH, Bazzoli GJ, Gerland AM. Hospitals’ responses to nurse staffing shortages. Health Affairs. 2006;25(4):W316–W323.
5. Duffield, C., Roche, M. A., Blay, N., & Stasa, H. (2011). Nursing unit managers, staff retention and the work environment. Journal of Clinical Nursing, 20 (1-2), 23-33. doi: 10.1111/j.1365-2702.2010.03478.x
6. Kumar S. Nursing Turnover – A Vibrant Problem in Healthcare Management: Costs, Causes, & Solutions. International Journal of Information Technology & Systems. 2012 June 7. 1 (1).
7. Cowden T, Cummings G, Profetto-McGrath J. Leadership practices and staff nurses’ intent to stay: a systematic review. J Nurs Manag. 2011 May;19(4):461-77. doi: 10.1111/j.1365-2834.2011.01209.x.
8. Becker S, McCutcheon H and Hegney D (2010). Casualisation in the nursing workforce-the need to make it work. Australian Journal of Advanced Nursing, 28(1): 45-51.
9. Sullivan C, Reading S. Nursing shortages: let’s be flexible. Collegian. 2002 Oct; 9(4):24-8.
10. Lundberg K. Promoting self-confidence in clinical nursing students. Nurse Educ. 2008 Mar-Apr;33(2):86-9. doi: 10.1097/01.NNE.0000299512.78270.d0.
11. Rawal CN, Pardeshi S. Job Stress Causes Attrition among Nurses in Public and Private Hospitals. Journal of Nursing and Health Science. 2014 Mar0 Apr: 3 (2); 42-47.
