Doctors are often cited as ‘God’ in healthcare setting. Ever wondered what happens when doctor leaves a patient, who is the constant source of energy, support and care. Answer isn’t a tricky one, it is the nurses who stand by the patients when in an ICU a patient is not happy with his meals and wants to have his juice exchanged as he doesn’t like the flavor or a patient who is disoriented and wouldn’t let anyone touch him is taken care by the nursing team.
“Number of Nurses had greater impact on patient at higher risk whereas the effect of medical staff remain unchanged”
West E, 2014
Surprising, isn’t it. But research says so. There are nurses who would go beyond their call of duty and cross a river full of crocodile to reach the people for treatment literally! Read story of Sunita Thakur, an ordinary nurse who changed the world around.

I am sure if you are in healthcare, you must have come across few of these heroes who either taught you how to give injection, stood there with you when you were delivering a baby for the first time or encouraged you as you performed an independent surgery all by yourself.
However derogatory the remarks would have been against nurses, we have all met and worked with some, who continue to work, thrive and make us proud of who we are- Nursing Professionals.
Patient outcome and journey in a health care set up is enormously impacted by the nursing care he/she receives. Whether it is an operation theatre where a nurse tells the surgeon to count the sponges and instrument so that there are no accidents or it is the post-operative nurse who quickly assesses, identifies a life threatening arrhythmia and informs the doctor on duty, it all matter. It will decide whether the patient will be re-admitted for an avoidable mistake or if the patient will suffer a complication and stay longer than expected in the critical care unit.
Difference between Morbidity and Mortality
Morbidity- Morbidity in literal sense means being sick, ill or unhealthy. When we describe it in terms of ‘increased morbidity’ it means the reference is deterioration or impairment of health which happens over time.
Mortality- Mortality is related to one’s risk of death. Usually mortality is described in number of deaths in a setting over time (say month/yearly).
Do nurses impact morbidity and mortality in healthcare?
Yes, the nurses have very critical role to play in patient outcome in terms of morbidity and mortality. Nurses provide patient care round the clock as a result they are in the best position to identify the early signs of any deterioration in patient condition and take action.
A large study done by Needleman et al found the link of increased patient mortality with low staffing.
Read more here: https://www.nejm.org/doi/full/10.1056/nejmsa1001025
Case Study: Readmission of Patient with Planned Appendectomy
Day 1: A patient 45 years old gets admitted for appendectomy. He is a smoker (1 pack/day) and has no other history of medical condition and is not taking any medications.
Day 2: Patient is received post procedure in the post-surgical unit after successful surgery with no complications. Vitals are stable. Patient is conscious and reports pain at the surgery site. Urine output at the end of the day is 1000 ml/ day.
Day 4: Patient is discharged from the hospital with precautions explained to him and follow up.
Day 5: Patient returns to the hospital complaining of breathlessness. Nurse starts oxygen at 5 l/min as oxygen saturation is 90% and informs doctor about the patient. Patient is monitored and assessed for any complication and surgery site. Saturation of the patient is maintained 98% to 100% and patient feels better. The patient reveals that he did not quit smoking just a day before the surgery as well and also suffered nasal congestion as he had infection.
The information in this case was missed by the health professionals as patient continued to smoke. Patient also failed to mention about the infection he suffered just before the surgery. In this condition, the surgery of the patient could have been postponed as this was not an emergency procedure. But, what happened?
Patient got readmitted and could have possible suffered a complication. This case study demonstrates the possible patient morbidity due to improper assessment and missed information. Not blaming anyone, it was the responsibility of both the doctor and the nurse. But as we know, nursing assessment is an important first step and many fragmented pieces of information which can be missed by doctors can be easily recovered if the nurse assesses a patient well. Knowledge and skill of the nurse does matter.
Morbidity and Mortality in healthcare and Role of Nurse
In healthcare setting there are certain group of complications whose outcome is impacted by nursing care the patient receives. These include the following:
Conditions that increase the morbidity rate at healthcare setting impacted by nurses
- Urinary tract infection
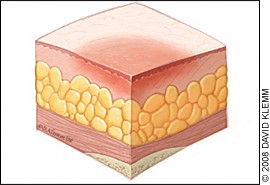
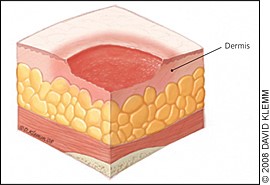
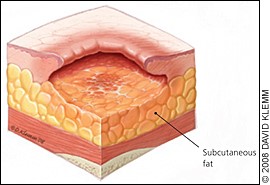
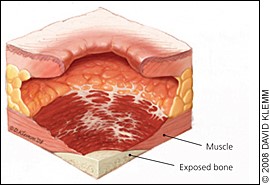
- Pressure ulcers
- Hospital acquired pneumonia
- Deep vein thrombosis
- Pulmonary embolism
- Procedure related upper GI bleeding
- Sepsis
- Shock
- Cardiac arrest
- Surgical wound infection
- Pulmonary failure
- Metabolic imbalances such as hypo/hypernatremia, hypo/hyperkalemia
Note that mortality rate in a hospital is increased as a result of failure to rescue due to above conditions which are the reason for higher morbidity.
Does increased staffing help prevent mortality and morbidity?
The answer is yes. Employing qualified nursing professionals as per the need of the unit is found to be related to patient outcomes and development of morbid complications that directly impacts the patient outcome.
There are many studies that support it. Nursing hours per patient day influenced patient outcomes tremendously. As per the literature the complications that were found to be directly impacted by staffing were:
- Urinary tract infection
- Pneumonia after surgery
- Thrombosis
- Pulmonary complications in surgery patients
- Medication errors
- Pressure ulcers
- Patient complaints
- Hospital acquired infections rate
- Mortality in healthcare setting
All these studies which found a direct relation between staffing and patient outcome also indicated that increased staffing was inversely related mortality rates, decrease mean length of stay and lower complications.
Does qualification of nurse impact morbidity and mortality?
Role of qualified nurses has long been recognized globally. A skilled nurse can judge and prevent adverse events in a unit. That’s why in many settings like post-surgical units, I have witnessed that the treating team relied more upon the nurses for patient progress in crucial hours. This is only possible if a nurse is qualified.
How do we define a qualified nurse? Does the degree matters?
Yes it does. A study indicated that 10% more B.Sc. nurses, decreased deaths and failures in among 665 hospital, regardless of their work environment, by roughly 4%.
Read more about the study here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217062/
Similarly, an extensive review of 27 studies done in 2018 says that higher levels of nurses’ education were associated with lower risks of failure to rescue and mortality in 75% and 61.1% of the reviewed studies pertaining to these adverse events. How qualified a nurse was also found to be associated with lowers hospital admissions and shorter length of stay.
Read more here: https://www.sciencedirect.com/science/article/pii/S002074891830018X
Other nursing factors impacting morbidity and mortality
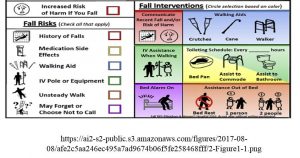
Nursing skill mix- Nursing skill mix means nurses are replaced with other staff like nurses’ aides and other assistant personnel and usually a cost control method employed by the hospitals. Arguments have also been there for more than a decade now where the nurses also support the employment of such personnel for certain tasks referred to as ‘Non-nursing tasks’. Twigg DE found that there was significant increases in three adverse events including failure to rescue, urinary tract infection and falls with injury where the assistant in nursing wards were placed with one significant decrease that is mortality.
Nursing skill mix has also been found to be associated with:
- Mortality
- Patient rating of hospital
- Nurse reported adverse events
It has been indicated that employment of temporary nurses are associated with increased mortality. The possible reason could be lack of orientation to the unit, understanding of protocols and accountability. Therefore, it is often been debated even in India with this trend that has recently come in to mix permanent with temporary nurses in certain setting including government set ups. Nurses have been protesting against it and demanding to absorb such nurses on permanent basis. The administration must understand that skill mix in this regard dilutes the quality of care a patient receives in any healthcare set up.
However, adding assistants to nurses who perform non-nursing tasks is appreciated as it prevents nurses’ burnout and let them concentrate on other tasks that are need more of their attention. The only way to ensure that the patient receives quality care even by these assistants is by educating them, training them and putting a set protocol which are monitored by quality nurses periodically.
Nurse- Physician Relationship- Believe it or not practical environment where a nurse works is found to impact how well care a patient receives. It also impacts nurses retention in a hospital. A good example that I quote from my own experience is in a tertiary care hospital, where neonatal ICU is managed by a great team of doctors and nurses. It is constantly been in top neonatal units in Asia. What is different? When I was gaining experience as a student in the unit, I saw a difference. The daily rounds of the consultant would include report of individual neonate from their respective assigned nurses. And as a student we were told by our peers to be extra prepared to answer questions that would be asked by doctors and nurses unequivocally. It was an experience I still cherish. Neonatal mortality has been magically controlled in this unit. Kudos to such team.
A study Siedlecki S, 2015 quoted that 55% of nurses said that physician’s behavior impact nursing decisions especially young nurses were affected more than older nurses. Similarly, Aiken LH also reported that hospital with better physician-nurse had lower 30-day mortality.
Happy Nurses Happy Patients
Nursing professionals to perform their best must be supported well. How can we do that?
- Know the nurses well who enter your organization. Use smart applications to assess them and understand their capabilities and place them accordingly. See link to know more: SMARTHIRE- https://play.google.com/store/apps/details?id=org.bodhihealthedu.smarthire
- Use acuity systems and distribute your nurses wisely.
- Promote individual endeavors. Support nurses to perform better by encouraging them to keep themselves updated and keep learning. You can enroll here: /product-category/nursingcourses/
- Promote professional interactions and follow evidence based practices.
- Teach and reinforce quality patient care with accountability. Educate nurses about the need, indicators and their role in preventing such events. Encourage them to monitor patient progress and publish their achievements.
- Teach assertiveness and encourage professional communication by setting an example by yourself. Learn more about here: /product/soft-skills-personality-types/
References:
1. West E. Barron DN, Harrison D, Rafferty AM, Rowan K, Sanderson C. Nurse staffing, medical staffing and mortality in Intensive Care: An observational study. International Jounral of Nursing Studies [Internet]. 2014 May [cited 2019 Mar 10]: 51 (5); 781-94.
Available from: https://www.sciencedirect.com/science/article/pii/S0020748914000340
2. Twigg DE, Myers H, Duffield C. Impact of skill mix variations on patient outcomes following implementation of nursing hours per patient day staffing: a retrospective study. Journal of Advance Nursing [Internet]. 2014 Feb 4 [cited 2019 Mar 10]: 2710-18.
Available from: https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1365-2648.2012.05971.x
3. Aiken LH, Sloan D, Griffiths P. Nursing skill mix in European hospitals: association with mortality, patient ratings, and quality of care. BMJ Qual Saf 2016;[Internet]. doi: doi:10.1136/bmjqs-2016-005567
4. Siedlecki S, Hixson E. Relationships between Nurses and Physicians Matter” OJIN [Internet]: 2015 Aug 31 [cited 2019 Mar 10]; 20 (3). DOI: 10.3912/OJIN.Vol20No03PPT03