“Nurse saves doctor after he collapses during a run.”
“Nurse saves gym-goer who collapsed after a heart attack.”
“An off-duty nurse was in the right place at the right time Sunday when a man suffered a medical emergency at a gymnastics event.”
The stories are endless and often go unnoticed how nurses save lives every day. But the question is, is it so easy to do so? Ever wondered how will you react if someone collapses in front of you? The quick response of any medical professional is “START CPR”.
But as a health professional how do you know whether the situation really needs you to start CPR or not. As nurses we are often the first responders to any emergency that happens in a hospital setting. As simple it sounds, if you do not know what and how to assess in a victim your brain could throw you off with many questions.
- Is it really an arrest?
- Does the victim really need CPR?
- What if I am not assessing the victim carefully and he is just asleep?
- What if I don’t perform CPR properly?
- Should I call a senior /Doctor first?
As scary it might sound, you do have very limited time to manage a collapsed victim and the more time one wastes, less are the chances of a survival. As per The Centers of Disease Control and Prevention (CDC), heart disease is the leading cause of death among men and women. We will address common misconceptions about CPR in this blog post.
Why should you learn CPR?
Nurses are the first responders– In a hospital, nurses need to manage an emergency before the team arrives.
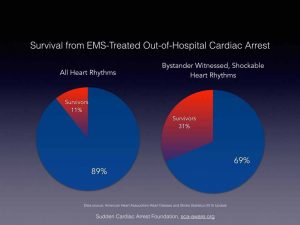
CPR saves lives– Cardiopulmonary Resuscitation is a simple life skills that not only save lives but also prevents long term complications such brain damage. According to American Heart Association (AHA), those victims who were treated by emergency medical services (EMS), 10.6% survived. Among the bystander witnessed cases in which individuals had a heart rhythm that could be treated effectively with a defibrillator, 31.4 % survived. The data reflects the importance of quick action taken by bystanders to save a life.
See link: https://www.sca-aware.org/sca-news/aha-releases-2015-heart-and-stroke-statistics
Source: https://www.sca-aware.org/sca-news/aha-releases-2015-heart-and-stroke-statistics
Increases your chances at a job- many job requirements specify nurses to be trained to perform and be certified as ‘CPR provider’. See the links below.
- American Heart Association BLS course- https://cpr.heart.org/AHAECC/CPRAndECC/Training/HealthcareProfessional/BasicLifeSupportBLS/UCM_473189_Basic-Life-Support-BLS.jsp
/product/cardio-pulmonary-resuscitation-cpr-adult/
Train others- Often nurses educators need to train others on essential skill of performing CPR. Nurse educators can go for higher certification and be trained as a trainer.
- American Heart Association Instructor course- https://cpr.heart.org/AHAECC/CPRAndECC/Training/AHAInstructors/UCM_476669_AHA-Instructors.jsp
Quality patient care- It is evident that if the nurses are well prepared to deal with the arrest situation in hospital and community, the patient care is bound to be better as they manage the situation effectively. American Heart Association stats that CPR, especially if administered immediately after cardiac arrest, can double or triple a person’s chance of survival. See more here:
https://cpr.heart.org/AHAECC/CPRAndECC/AboutCPRECC/CPRFactsAndStats/UCM_475748_CPR-Facts-and-Stats.jsp
When should be CPR performed?
Cardiopulmonary Resuscitation should be performed when someone is not breathing or when the heart stops beating. In many situations the victim might not be a cardiac patient or have a history of cardiac disease. One should know that there may be other situations as well where a victim might experience cardiac arrest or stop breathing, this include the following conditions.
- Stroke or tumor
- Choking
- Allergic reaction
- Traumatic injury (head/neck)
- Electric shocks
- Drowning
So, CPR must be performed in any situation when a person in not breathing or has no pulse.
What is the difference between CPR and First aid?
First aid refers to the initial action taken by the responders in case of an emergency situation.
So how is CPR different from first aid?
First aid teaches the res-ponders to recognize a variety of emergency situations such as head injuries, neck injuries, burns, traumatic injuries whereas CPR is a ‘step’ while providing first aid in case a victim suffered cardiac arrest, near drowning situations or when the victim is not breathing.
Read more about CPR and First Aid courses here:
- American Heart Association CPR and First Aid Training Classes-https://cpr.heart.org/AHAECC/CPRAndECC/FindACourse/UCM_473162_CPR-First-Aid-Training-Classes-American-Heart-Association.jsp
- American Red Cross- https://www.redcross.org/take-a-class/first-aid
Steps of First aid during arrest situation include:
1. Call for help- Call on emergency number.
2. Provide First aid- There can be a number of reasons if the person stops breathing or the heart stops. For example traumatic injury or choking. If the victim has suffered an arrest situation, the rescuer must provide initial first aid such as performing Heimlich maneuver or removing the victim from the danger zone. See the link to know more about Heimlich maneuver here.
3. Start CPR- Start CPR as soon as possible as time to avoid complications of injuries to get worsen.

Source: http://boostafosterfamily.org/wp-content/
Methods of performing CPR
1. CPR by trained health professionals- It is recommended that trained health professionals should check for pulse and start CPR if no pulse can be felt within 10 seconds starting with chest compression. Start 30 chest compressions followed by 2 rescue breaths.
Learn about CPR for health professionals here:
Cardio Pulmonary Resuscitation (CPR)-Adult
Cardio Pulmonary Resuscitation (CPR)-Infant
2. Hands only CPR/CPR without ventilation- If you are not trained in performing CPR or you have not renewed your certification within two years, it is suggested that one must perform hands only CPR that is provide chest compressions only. The rescuer only provides chest compression without giving ventilation to the victim.
What are the steps of CPR?
The steps of CPR were revised and changed from ‘A-B-C’ to ‘C-A-B’. The evidence suggest that chest compressions is the most important step during CPR than opening airway and breathing in adults. Thus, it is recommended that the rescuer must begin performing chest compression and then focus on airway and breathing.
C stands for Chest Compression
A stands for Airway
B stands for Breathing
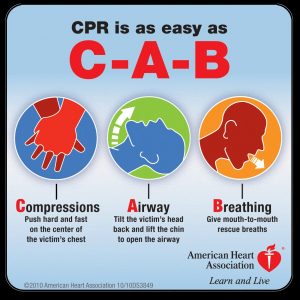
Source: https://medictests.com/abc-vs-cab-correct/
CPR using Automated External Defibrillator (AED)
CPR is crucial for the survival of an individual who has suffered an arrest, but often use of AED is equally emphasized. Automated External Defibrillator or AED is a device suggested to be used as soon as it is available. AED are placed in public places and are meant to be used if an arrest situation happens at a public place. AED can identify the abnormal heart rhythm and decides whether shock needs to be given or not. An AED gives instructions from pushing the button to connecting the pads. The purpose of AED is that, even a layman or untrained professional can give shock to the victim saving a life without causing damage. It has been proven that early shock increases the chances of survival of a victim. Learn more about how to use an AED here.
Automated External Defibrillator
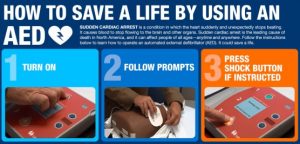
Source: https://i1.wp.com/scrubbing.in/wp-content/uploads/2013/09/AED.png?resize=556%2C266
CPR with defibrillator
Defibrillator is device that gives shock to the heart when life threatening arrhythmia such as Ventricular tachycardia and Ventricular fibrillation occurs. These are the only two conditions where a defibrillator is used. Health professionals must use a defibrillator as soon as it is available. It is preferred to use a manual defibrillator than AED if both are available.
In case you are unsure of the dose of defibrillator remember the following practical points:
- Know your defibrillator- Check what type of defibrillator is available in your unit. For example if it says ‘Monophasic’ then the amount of energy requirement is more (360 J). If the defibrillator is ‘Biphasic’, you can start with lower energy (120 J, 150 J).
- Be consistent- This means if you started at a dose of 150 J give the next shock with same amount of energy.
- Increase the energy with each shock- You can either choose to give same amount of energy with each shock or you must increase the dosage with each shock (120 J, 150 J and 200 J).
Learn more about using defibrillator on the following links:
CPR without defibrillator
Do you always need a defibrillator when resuscitating a victim? The answer is No.
You don’t always need a defibrillator during an arrest situation. While providing first aid to a person who has collapsed, the most important thing is to start CPR. By providing chest compressions, you are manually trying to pump the blood from the heart to the other organs of the body. This act ensures that the vital organs are still getting oxygen through blood. Defibrillator temporarily stops the heart rhythm and allows the heart to resume back the normal rhythm. There are certain conditions where you do not need a defibrillator during CPR which include Pulse-less electric activity and asystole. In these conditions, the heart has ‘no rhythm’, so giving a shock will not be of any benefit. Only thing that can save life in such conditions is CPR.
If you are using an AED it will instruct you to continue CPR and not give any shock but if you are using a manual defibrillator you need to recognize these conditions on your own.
Steps to be a confident CPR provider
1. Learn the basics- Pay attention to important steps and principles behind them for example C-A-B sequence, chest compression quality and pulse check. Learn more about the basics here: Bodhi Link
2. Know the medications- Nurses are expected to provide IV medication during resuscitation. Read about medications and recommended dosage in various arrest situations. For example epinephrine is the drug of choice irrespective of the heart rhythm during a cardiac arrest.
3. What not to give- Be updated what actions or drugs not to give during resuscitation. For example atropine is no more used during arrest situation. American Heart Association stopped recommending atropine during cardiac arrest since the guidelines released in 2010. Learn more about the changes here: http://www.heart.org/idc/groups/heart-public/@wcm/@ecc/documents/downloadable/ucm_317350.pdf
4. Orient yourself to emergency equipment- Keep yourself updated with the emergency or crash cart to understand the placement of drugs, equipment like ET tube, defibrillator, laryngoscope which are used during resuscitation.
Learn more about what items to expect in a crash cart here:
5. Refresh knowledge and skills- Participate in BLS and ACLS courses after a minimum duration of two years to renew your knowledge and skills of performing CPR.
CPR courses for nursing professionals
Nurses can undergo variety of certificate courses based on their area of placement and professional requirements.
Cardio Pulmonary Resuscitation (CPR)-Adult in English
Cardio Pulmonary Resuscitation (CPR)-Infant in English
American Heart Association Advance Cardiac Life Support-
American Heart Association Pediatric Life Support-
CPR certification Vs Re-certification
CPR certification lasts for a duration of two years. Researches indicate that there is deterioration of knowledge and skills of performing resuscitation with time. American Heart Association suggests that the health professionals must undergo re-certification to refresh the knowledge and skills of performing CPR every two years. Re-certification might take lesser time compared to the initial certification depending upon the organization you choose to certify yourself with.
You can choose to go for a blended learning and e-learning. See link:
https://www.redcross.org/take-a-class/cpr/cpr-training/cpr-renewal
NOTE: Make sure the certification you choose to undergo is recognized by your employer.
Conclusion
In many organizations and units where nurses work, CPR is an essential skill which they must be trained in such as emergency department and critical care units. It is a crucial skill which nurses must learn and encourage others as well to learn, as it not only helps them at the professional front but also empower them to be ready for adverse events that might happen at home and other social settings. See more inspiring stories here and learn more about CPR heroes:
https://www.bhf.org.uk/how-you-can-help/how-to-save-a-life/what-is-cpr/everyday-heroes
“Take Action- Learn CPR”
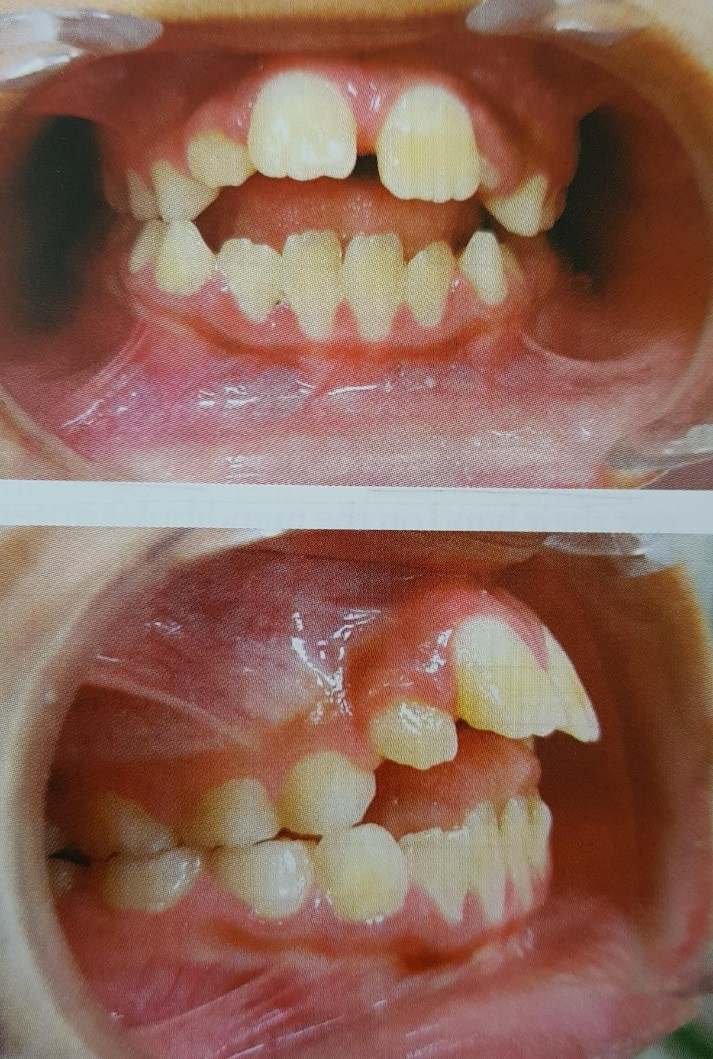
 Palatal crib
Palatal crib  blue grass appliance
blue grass appliance